|
Healing mental health disorders is a multifaceted journey that requires addressing the diverse and interconnected factors contributing to an individual’s well-being. The bio-psycho-social-spiritual model provides a comprehensive framework for understanding and treating mental health issues, emphasizing the importance of integrating biological, psychological, social, and spiritual dimensions. This holistic approach ensures that treatment is personalized and addresses the unique needs of each individual, fostering a more effective and enduring recovery process.
Biological aspects of healing involve medical interventions such as medication and lifestyle changes that can significantly impact mental health. For instance, medications like antidepressants or antipsychotics can help regulate neurochemical imbalances, providing stability for individuals to engage more fully in their healing journey. Additionally, lifestyle modifications such as movement, mindfulness, and adequate sleep are crucial in supporting overall brain health and reducing symptoms of mental health disorders. These biological interventions are often most effective when combined with other therapeutic approaches. Psychological, social, and spiritual healing are equally vital in the recovery process. Psychological therapies, such as dialectical behavior therapy (DBT), help individuals develop healthier relationship patterns and emotional expression. Trauma, somatic and polyvagal therapies help to regulate the nervous system. Increasing social support, building strong relationships with family and friends and involvement in community activities, provides a sense of belonging and reduces feelings of isolation. Supporting spirituality, whether through religious practices, meditation, or a personal sense of purpose, can offer profound comfort and resilience. By nurturing all these dimensions, individuals can build a robust foundation for healing, creating a life filled with hope, connection, and meaning. Meeting with a skilled and sensitive mental health therapist can support each and/or all of these dimensions of a person’s mental health, diminishing, and sometimes eliminating, the effects of mental health disorders.
0 Comments
When discussing Post-Traumatic Stress Disorder (PTSD) with clients in the aftermath of their traumatic experience, we have noticed a recurring experience. Many times, clients who meet criteria for the diagnosis of PTSD understand this to mean that they will always suffer from the effects of their trauma. All too often, we see a shadow sweep over our client’s faces as shame and fear rise in their bodies. We want to help clarify this particular diagnosis with a message of hope. PTSD is not a lifelong chronic condition, rather a description of how our bodies work to restore safety after trauma. Let’s talk about Post Traumatic Stress and how we can use this information to work toward healing.
Post-traumatic stress (PTS) is a natural response to experiencing or witnessing a traumatic event, impacting both mind and body. When confronted with trauma, the body's nervous system initiates a complex cascade of responses aimed at survival. Understanding the neurobiological impact of trauma can shed light on the symptoms individuals may experience, such as hypervigilance, flashbacks, and emotional dysregulation. Understanding PTS must involve the nervous system's role in trauma, which illuminates how our body reacts to perceived threats. Traumatic experiences can dysregulate the autonomic nervous system, leading to a state of hyperarousal or dissociation. This dysregulation can disrupt the body's ability to distinguish between real and perceived danger, resulting in ongoing feelings of fear and vulnerability. By learning about the nervous system processes at play, individuals can gain insight into their symptoms and recognize that they are not signs of weakness but rather adaptive responses to overwhelming circumstances. This knowledge can also inform treatment approaches, emphasizing interventions aimed at regulating the nervous system's stress response. Treatment for PTS often involves therapeutic modalities that target both the mind and body. Polyvagal theory helps to pay attention to nervous system signals and to use this information to create safety in the mind and body. Dialectical Behavior Therapy (DBT) helps individuals become skillful in mindfulness, emotional regulation, interpersonal skills and distress tolerance, while somatic experiencing focuses on releasing stored trauma from the body. Eye Movement Desensitization and Reprocessing (EMDR) and Brainspotting harness the brain's natural healing mechanisms to reprocess traumatic memories and alleviate distress. These approaches not only address psychological symptoms but also aim to restore balance to the nervous system. Despite the challenges posed by PTS, there is hope for recovery. With the right support and resources, individuals can learn to regulate their nervous system responses, reduce symptoms, establish safety and cultivate resilience. It's essential to approach treatment with compassion and patience, recognizing that healing is a gradual process that unfolds over time. In conclusion, understanding the neurobiological impact of trauma is crucial for navigating post-traumatic stress with compassion and efficacy. By integrating this knowledge into psychoeducation and treatment approaches, we can empower individuals to reclaim agency over their healing journey. Remember, recovery is possible, and there is hope for a brighter future beyond trauma's shadow. Next week’s blog post will be about Post Traumatic Growth. Introducing Radical Acceptance Radical Acceptance is a core skill in Dialectical Behavior Therapy (DBT). This skill falls into the category of Distress Tolerance skills. We reach for this skill when we are navigating something big and hard in our life that is outside of our control or influence. The idea behind Radical Acceptance is that we can work to improve our wellbeing even in the midst of the big and hard things. To appreciate what Radical Acceptance can offer us, we must first understand the difference between pain and suffering. Pain is an inevitable part of being human in our world. We will all experience pain at different times in our life. Suffering, however, is caused when we make choices that make painful circumstances harder for ourselves. Radical Acceptance seeks to accept pain and reduce suffering. When we reduce suffering, we grow in emotional resilience and wellbeing. Understanding Radical Acceptance Radical Acceptance is the act of fully acknowledging and embracing reality without judgment or resistance. In other words, Radical Acceptance is a choice to stop fighting against reality. Likely something is happening in our life that is hard and beyond our ability to change it, and we are left with the decision to accept (radically) or reject the reality of the situation. The radical part of Radical Acceptance speaks to the complete and total nature of our choice to accept reality. Radical Acceptance is not resignation or apathy, rather it is a conscious choice to yield to what is real. Radical Acceptance also does not require our stamp of approval on the difficult circumstances, instead a simple acknowledgement that it exists and that we will stop fighting against it. Suffering comes when we fight against painful events that we don’t have the power to change, and Radical Acceptance offers us a peaceful alternative. Cultivating Radical Acceptance DBT offers us some step-by-step guidance on how to execute the choice to Radically Accept painful circumstances.
We can draw upon other DBT skills as tools to help us in this process. Mindfulness skills help us notice what is happening internally and externally and bring awareness to the present moment. Additionally, mindfulness skills call us to self-compassion and nonjudgmental observation of emotions. We may have an opportunity to reframe negative thoughts about our reality and notice growth opportunities or unexpected benefits. Some nourishing activities like journaling and spending time in nature can help promote acceptance. Often times, Radical Acceptance requires patience and practice, as most painful events will require us to choose acceptance over and over again. Disclaimer: Radical Acceptance is not an excuse for harmful or abusive dynamics, but it may be a starting point for being honest about the harm that exists. May this honesty open doors for healing and support. Written by Allison Harvey
Trauma survivors have gone through something that challenged every part of them, most significantly their sense of safety. Their needs are personal, unique to their personality and circumstances, and often quite delicate. Naming these needs creates space for trauma survivors to feel safe, work toward healing and maintain connection with loved ones. Physical Needs On a very basic level, trauma survivors have a need for safety and security. Through their traumatic incident(s), they learned to be on guard and watchful. Trauma survivors need a physical location where they can let their guard down and rest. Trauma survivors also need access to medical and psychological care—professionals to come alongside them and nurture their physical and emotional self back to health. Trauma survivors also need adequate nutrition and sleep. Tending to these basic needs helps to heal a nervous system that felt a strong lack of safety. Emotional Needs Those who have survived trauma(s) have a strong need for emotional understanding, empathy and validation. When they are ready to share about their story, they need to be received with compassion, support and validation that says “what you are feeling makes sense to me.” Trauma survivors can also be supported with emotional skills that help them navigate trauma triggers and a large emotional burden while they are healing. Social Needs Trauma healing happens within a safe, understanding and supportive relationship(s). Those who have survived trauma need their people to remain open to them. Trauma healing can be messy and indirect, so survivors need compassion and grace to learn to feel safe in relationships again. Survivors may need more accommodations so that they can stay regulated, and this may look like them setting boundaries or asking for certain changes. Connecting with others who are healing from trauma can be very beneficial as well. Psychological Needs Professionals who are supporting trauma survivors should be trauma-informed and have a path toward healing in mind. Psychological care should be gentle and paced by the survivor. Professionals should respect the trauma survivor’s wishes to tell their story or not, knowing that healing can happen either way. Trauma survivors benefit greatly from learning and practicing coping mechanisms and stress management techniques. All of these activities support the survivor to rebuild trust, regain resilience and personal strength. Practicing this DBT Skill can help us stay grounded and connected this holiday season! Mindfulness is a skill that, when practiced regularly, is a great tool to reduce stress, connect with our personal goals and create genuine connection with others. The holidays can be rich in memory, sentiment and relationship. They can also be full of family expectations, grief and reminders of trauma. These, and many more experiences, can overwhelm, cause us to disregard our own needs, and flood us with many different emotions. In order to enjoy the positive aspects of the holiday and skillfully navigate the challenges, try practicing mindfulness throughout your holiday season!
Mindfulness has three components:
Mindfulness as Stress-Reduction For many, the holiday season means a busy schedule and many more tasks and to-dos than normal. Practicing mindfulness in the midst of the whirlwind helps to produce moments of calm to catch our breath and remember our priorities. Mindfulness also helps us evaluate where our time and energy are going and make the most intentional decisions for ourselves in this season. Mindfulness as Social Support Paying attention to the present moment, without judgement can give us a lot of important information about what is happening in a room, or in a conversation. In the midst of a holiday gathering, take a moment to simply observe what is happening inside and outside of yourself. Allow yourself the gift of a few deeper breaths. Notice who is talking with who, and what those dynamics are like. Notice what is happening inside yourself as you connect with different people. Hold this information lightly and without judgement, and allow this information to guide your interactions. Mindfulness to support Intentional Decisions If you find yourself navigating a lot of spoken and/or unspoken expectations over the holidays, mindfulness skills can help you identify your needs and desires and to stay connected to them throughout the season. Spend some intentional moments noticing where you would like your time and energy to go this season, what would make it memorable and special for you and yours. Notice how other’s expectations are making you feel, especially if those expectations cause you to disregard your own needs and desires. Give yourself the gift of staying connected to yourself and your values, which becomes a much more congruent and grounded holiday experience. Dialectical Behavior Therapy (DBT) offers a set of skills to help with many different emotional and relational difficulties. The four pillars of DBT are Mindfulness, Emotion Regulation, Interpersonal Effectiveness and Distress Tolerance. Each of these pillars offers a number of skills to practice in that area. I have selected three DBT skills that I believe can make a significant difference for those managing depression.
Depression is an experience that includes a slow-down or freeze response in the nervous system. People managing depression may feel numb, detached, hopeless and sad. These internal experiences may cause them to isolate from relationships, get stuck in their difficult emotions, struggle to complete normal activities. Often, those managing depression feel misunderstood by the people in their life, especially when they are encouraged to “think positively” and “just get over it.” In fact, people managing depression are often expending enormous effort to engage in their life in the most simple ways. The following set of DBT skills can be used together or individually to improve depression symptoms and help catalyze healing and forward movement. 1.Emotion Regulation Skill: Opposite Action When we are using Emotional Regulation skills, we are paying attention to whether or not our emotions fit the situation we are in. Opposite Action is a skill that we reach for when we have determined that our emotions DO NOT fit the facts of the situation. This is often the case with depression. Depression is like a lens that makes life look harder and sadder than it actually is. All emotions have an action urge, an instinctual action that the emotion makes us want to do. When our emotions DO NOT fit the situation, we benefit from acting opposite to the action urge. Here are some common emotions experienced in depression and suggestions for opposite action.
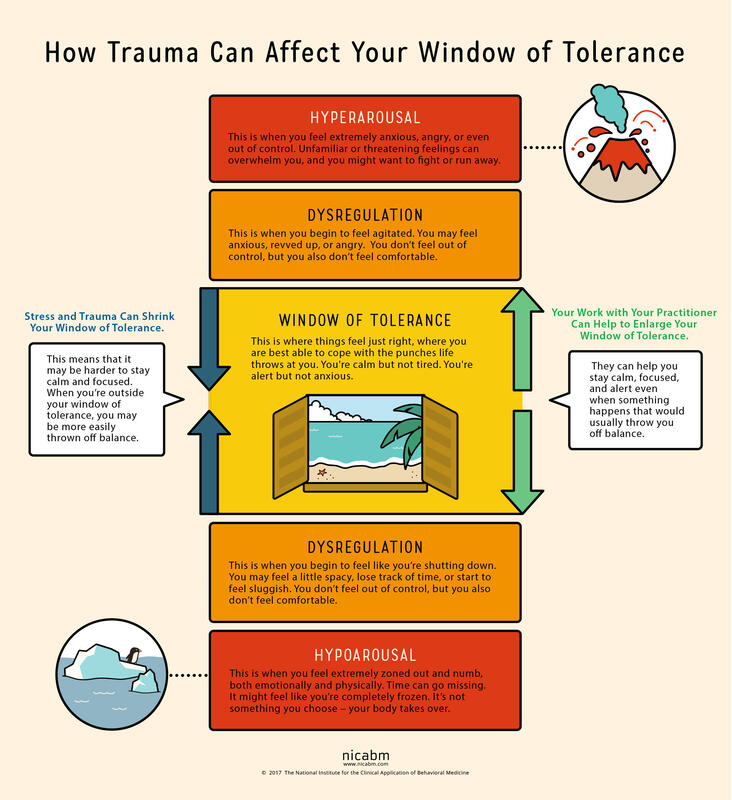
2.Interpersonal Effectiveness Skill: Making Requests Making Requests is a relationship skill that is very closely related to making boundaries. Requests highlight what we need from another person. While they can be vulnerable to make, they are also vital to communicating our needs with others. Loved ones are not mind-readers and need invitations and instructions to know how to care for those managing depression. People experiencing depression are almost always misunderstood by the people who care for them most. Unless they have experienced depression themselves, loved ones will likely minimize the depressed experience. From the outside, it may appear that it would only take a few simple steps to recover from depression. If only that were true. In order to stay connected with loved ones and to receive the care they absolutely need, those managing depression need to lean into this skill of making requests. They need to speak about how they are feeling and the effort they are expending to engage with their lives. They need to ask their loved ones to be patient with them, to use encouraging language, to offer comfort and presence rather than solutions. 3.Distress Tolerance Skill: Radical Acceptance We reach for distress tolerance skills when we are going through circumstances that are too big and/or too hard for us to change. Depression often comes on the tails of a big and hard life event, such as the loss of a loved one, a difficult transition, a painful event or unmovable circumstances. When there is truly nothing we can do to change our circumstances, we need to shift our focus toward acceptance. We are using radical acceptance skills when we work to create openness and willingness toward our difficult circumstances. Willingness is a powerful mindset shift and means that we will stop fighting against what is inevitable. Endlessly fighting against unfavorable circumstances is a recipe for suffering. Pain is inevitable in our lives, but suffering is a choice. We can still live meaningful lives in the midst of painful circumstances. When we give up the fight, we are more able to find acceptance. . . and peace. Living with depression can be a completely consuming experience. Those experiencing depression can have symptoms like persistent sadness, hopelessness, lethargy, low self-esteem, guilt, worthlessness, and more. These symptoms exist on a spectrum from mild to severe and short to long-term. Living day to day with depression feels heavy, aimless and dark. Often people suffering from depression are told to change their mindset in order to recover. We know that change must come from a much deeper place. In fact, living day to day with depression requires enormous amounts of courage and perseverance, and it helps those who are suffering to have this acknowledged and validated. Depression has several different causes and sources. There are strong inherited patterns for major depression. There are also significant hormonal impacts, especially in post-partum depression and pre-menstrual depressive disorder. Personality also has a strong influence on mood and energy and motivation. All of these different also create causes can also produce a predisposed sensitivity to depression. This blog post is to highlight when life circumstances or traumas are the source of depression. When this is the case, it is the nervous system that is leading the body and mind toward depression. And as such, treatment will need to be focused on healing the nervous system and helping the client work toward a different nervous system state. When the nervous system (read: trauma, overwhelm, life circumstances) is causing depression, healing must happen deeply in the autonomic (involuntary) nervous system. To understand the nervous system impact and the healing of nerves, we need to understand the Window of Tolerance. When we are in the window of tolerance, we are grounded, flexible and able to roll with the ups and downs of life. When we have a good amount of resilience, our window of tolerance is large and we are able to handle significant challenges without becoming too dysregulated. When we are under a lot of stress, our window of tolerance shrinks and we start to experience hyper or hypo arousal. Let’s discuss these nervous system states that exist outside of the window of tolerance. When we experience overwhelming stressors, we become dysregulated in one of two different directions, sometimes cycling between the two. We can become activated and have a flood of anxious or angry energy wash through our body (hyperaroused). Or we can become deactivated and experience numbness and a shut down response (hypoarousal). This hypoaroused state is the embodiment of depression. This is how stressors or traumas cause depression.
Hypoarousal symptoms also exist on a spectrum. On the milder side, we might experience tiredness, brain fog and a slump in energy. When hypoarousal is heightened, one might experience emotional numbness, dissociation, and even catatonia. Sometimes, we end up in this depressed state after an extended period of stress. It’s like our system is saying that it can’t handle that level of activation for that long and it shuts down. In other words, depression can be caused by a nervous system shut down. So, what does our nervous system need when it is in this shut down state? Sometimes, it simply needs a break. It needs rest from the hyper-activated state. The nerve that runs these activation pathways has become raw and overworked and needs to be soothed. The nervous system also has a significant need for connection when it is in this state of shut down. It needs a form of connection that is accepting, supportive and understanding. The nervous system also needs a way to process or integrate the overwhelming emotions that shut it down in the first place. This typically needs to happen at a slow and measured pace, so not to overwhelm again. These interventions serve as a ladder that helps us climb out of the shut down state, closer and closer to that window of tolerance. For a sustained healing process, we also need to take a good look at our lifestyle. When healing from a nervous system shut down, we need to choose a gentle pace of life, avoiding any additional stressors when possible. We can boost our nervous system health with meditation and mindfulness skills. We can invest in sustainable sleep habits that allow our entire system to regenerate every night. Gentle, joyful movement practices can also lift us out of shut down or depression. We at Benediction honor your nervous system and it’s inherent needs and functions, and we know how to move you out of harmful nervous system pathways. We can help you reconnect with yourself and with others by bringing your system back into balance in that lovely window of tolerance. Social anxiety can be consuming and can really limit the life experiences one might be open to. Imagine having to overcome a wave of panic, accompanied with rapid heartbeat, muscle tension and even blurry vision when walking into certain social circumstances. This dizzying experience can feel disorienting and even dissociative. When this happens regularly, it is understandable that we might start to avoid situations that cause this response all together. When this becomes a pattern, we may experience a narrowing of life experiences, a decrease in self-esteem and a reduced willingness to try new things.
It is possible to learn skills that help us navigate social events with more ease. Feeling confident and calm in social situations allow us to be present with ourselves and with others in the room. We are more able to be genuine and operate within our natural personality, making higher quality connections. There is one skill that has been the most helpful for our clients who are unlearning social anxiety. It is the DBT Mindfulness skill OBSERVATION. To understand this skill the most, let’s take a quick look at Mindfulness. When we are practicing mindfulness, we are 1) noticing our internal/external environment,2) without judgement and 3) without minimizing or enhancing what we find there. It is simply a practice of noticing. Noticing what we are feeling in any given moment. Noticing what is happening around us. Noticing what might feel like a threat. Simply noticing. Mindfulness practices like this slow us down and bring us into the present moment. And when we break this mindful practice into even smaller skills, one of the most impactful skills is that of OBSERVATION. We are simply taking in information, through our senses, thought processes and relationships. To observe skillfully, we need to create enough distance from what we are encountering to fully take it in. And this observable distance can make a big difference for social anxiety. Let me explain a little more clearly. Imagine yourself preparing to go to a social event where you do not know anyone. You are expecting to walk into a room of people milling around and forming small conversation groups, and you are expected to go and have a good time. Practically speaking, this might be a business networking event, an awards ceremony, a college orientation day, etc. What I am encouraging you to try, is to enter the event as an OBSERVER first and foremost. Find a comfortable place in the room to sit or stand. Once you are there, take a few deep breaths that bring you into the present moment and allow the room to stop spinning. As you do this, you are creating an observable distance from which you can take in all that is happening in the room in that moment. Notice what is happening around you. Notice how many conversation groupings there are, how are the people in conversation feeling, are there other nervous people present, where are the food and beverages located, are there people who are also looking for someone to talk with? You are simply noticing what is happening in the room. And from this observation point, you might start to notice where you’d like to be in the room. You may prefer to stay right where you are at, you may notice a conversation you’d like to join, you may notice that you’d like to get a drink before doing anything else. Regardless of where you go from here, mindfully observing your surroundings has allowed you more choice to be genuine in your interactions. And with practice, you may just feel more open and confident in new social situations! |
Archives
July 2024
Categories
All
|

 RSS Feed
RSS Feed