|
Understanding the origin of mental health disorders involves examining a complex interplay of various factors that can influence an individual's mental well-being. One of the most comprehensive models used to understand this complexity is the bio-psycho-social-spiritual model. This approach recognizes that mental health is not solely the result of biological factors, but also includes psychological, social, and spiritual dimensions. Each of these areas can contribute to the development of mental health disorders, making it essential to consider the whole person in treatment and prevention efforts.
Biological factors play a crucial role and include genetics, neurochemistry, and physical health conditions. For instance, research has shown that certain mental health disorders, such as depression and schizophrenia, can run in families, suggesting a genetic component. Neurochemical imbalances, such as deficiencies or excesses in neurotransmitters like serotonin and dopamine, are also linked to various mental health issues. Biological factors can serve as a pre-disposition to mental health disorders and become expressed in the presence of stress or trauma. Additionally, physical health problems, chronic illnesses, and even prenatal factors can influence mental health, underscoring the need for a holistic approach to healthcare. The psychological, social, and spiritual dimensions are equally significant. Psychological factors include one's emotional state, coping mechanisms, and past trauma or experiences. Social factors encompass relationships, community support, and systemic oppression, which can profoundly impact one's mental health. For instance, relationship distress or financial uncertainty can exacerbate mental health issues. Lastly, the spiritual dimension involves an individual's sense of purpose, beliefs, and connection to something greater, which can provide resilience and a sense of peace. By addressing all these aspects, individuals can achieve a more balanced and fulfilling life, fostering hope and recovery in the journey towards mental well-being. Stay tuned for next week’s blog about hope for healing mental health disorders.
0 Comments
The mental health needs of LGBTQ+ individuals are unique and complex, often shaped by the distinct challenges they face in society. Discrimination, stigma, and the pressure to conform to heteronormative and cisnormative expectations can create an environment where LGBTQ+ people are more susceptible to mental health issues. Studies show that LGBTQ+ individuals are at a higher risk for depression, anxiety, and suicidal ideation compared to their heterosexual and cisgender counterparts. These elevated risks underscore the importance of providing tailored and sensitive mental health support that acknowledges and addresses these specific challenges.
One critical aspect of supporting LGBTQ+ mental health is understanding the impact of minority stress. Minority stress refers to the chronic stress experienced by individuals from stigmatized minority groups. For LGBTQ+ individuals, this stress can stem from various sources, including internalized homophobia or transphobia, experiences of discrimination, and social rejection. Such stressors can profoundly affect mental health, leading to feelings of isolation, low self-esteem, and chronic anxiety. Mental health professionals need to be aware of these factors and incorporate them into their therapeutic approaches, creating a safe and affirming space for LGBTQ+ clients. Healing the nervous system is a vital component of mental health care for LGBTQ+ individuals. Chronic stress and trauma can dysregulate the nervous system, leading to symptoms such as hypervigilance, anxiety, and emotional numbness. Techniques that promote nervous system healing, such as mindfulness, deep breathing exercises, and somatic therapies, can be particularly beneficial. These practices help individuals reconnect with their bodies, release stored tension, and cultivate a sense of safety and calm. By integrating nervous system healing into mental health care, therapists can help LGBTQ+ clients build resilience and recover from the impacts of trauma. Moreover, social support plays a crucial role in the mental well-being of LGBTQ+ individuals. Building and maintaining connections with affirming and supportive communities can mitigate the negative effects of minority stress. LGBTQ+ support groups, community organizations, and online forums can provide safe spaces for individuals to share their experiences, receive validation, and find solidarity. These connections not only reduce feelings of isolation but also empower individuals to embrace their identities with pride and confidence. Encouraging LGBTQ+ individuals to seek out and engage with supportive communities can significantly enhance their mental health and overall well-being. Ultimately, a compassionate and holistic approach to mental health care is essential for LGBTQ+ individuals. By addressing the unique challenges they face, promoting nervous system healing, and fostering supportive social connections, we can create an environment where LGBTQ+ individuals can thrive. Mental health professionals, allies, and communities all play a crucial role in this process. Through understanding, empathy, and proactive support, we can help ensure that every LGBTQ+ person has the opportunity to live a fulfilling and mentally healthy life. "Traumatic events are extraordinary, not because they occur rarely, but rather because they overwhelm the ordinary human adaptations to life."
- Judith Herman, Trauma and Recovery When you hear the word, "trauma," what comes to mind? Growing up, I placed trauma in a category of things I only heard about on the news. Events like plane crashes, robbery at gunpoint, or natural disasters made sense to me. Of course they were big and terrible and traumatic--the news said so! However, as I got older, I realized that there was much more grey area about what was actually considered trauma or not. Some trauma is publicized, but other times thoughts about it can become so difficult that even one's closest friends do not know about it. Furthermore, trauma to one person may not be considered trauma to another. In these cases, is it still considered trauma? While some trauma can take a very clear and pervasive form, like in the cases I mentioned above, it can also be more subtle and even happen over a period of time. Often, individuals do not seek out the counseling treatment they need because they do not feel like their experiences were "bad enough." If you are wondering if you have experienced trauma and should consider counseling, I recommend asking yourself two questions. First, do you have experiences in your life that you would define as traumatic? I'm not asking whether your aunt or the newspaper or your Facebook feed calls it traumatic. Instead, I want to know how YOU feel about your experiences. If you have experienced an event in your life that you define as traumatic and want to talk about it, I would urge you to consider calling a counselor. You may be surprised by how healing it is to have your story of trauma validated by an objective individual. Perhaps you are certain you have experienced trauma, but still do not know if you should consider counseling. In that case, my second question to you is this: are you having difficulties in life that you did not have before the trauma occurred? For example, you may find that you struggle to sleep through the night, have an increased/decreased appetite, or have difficulty completing tasks efficiently at work or school. Or maybe the experience of the trauma has become so pervasive that you can't seem to stop thinking about it. By seeing a counselor, you can begin to develop coping skills that will reduce your post-traumatic symptoms and help you feel more functional in your daily life. If you can answer yes to one or both of these questions, it may be time to consider reaching out for trauma therapy. Healing is possible when you are willing to commit the time to properly honor your story in the context of a safe relationship. Written by Christian Swan on March 09, 2017 Practicing this DBT Skill can help us stay grounded and connected this holiday season! Mindfulness is a skill that, when practiced regularly, is a great tool to reduce stress, connect with our personal goals and create genuine connection with others. The holidays can be rich in memory, sentiment and relationship. They can also be full of family expectations, grief and reminders of trauma. These, and many more experiences, can overwhelm, cause us to disregard our own needs, and flood us with many different emotions. In order to enjoy the positive aspects of the holiday and skillfully navigate the challenges, try practicing mindfulness throughout your holiday season!
Mindfulness has three components:
Mindfulness as Stress-Reduction For many, the holiday season means a busy schedule and many more tasks and to-dos than normal. Practicing mindfulness in the midst of the whirlwind helps to produce moments of calm to catch our breath and remember our priorities. Mindfulness also helps us evaluate where our time and energy are going and make the most intentional decisions for ourselves in this season. Mindfulness as Social Support Paying attention to the present moment, without judgement can give us a lot of important information about what is happening in a room, or in a conversation. In the midst of a holiday gathering, take a moment to simply observe what is happening inside and outside of yourself. Allow yourself the gift of a few deeper breaths. Notice who is talking with who, and what those dynamics are like. Notice what is happening inside yourself as you connect with different people. Hold this information lightly and without judgement, and allow this information to guide your interactions. Mindfulness to support Intentional Decisions If you find yourself navigating a lot of spoken and/or unspoken expectations over the holidays, mindfulness skills can help you identify your needs and desires and to stay connected to them throughout the season. Spend some intentional moments noticing where you would like your time and energy to go this season, what would make it memorable and special for you and yours. Notice how other’s expectations are making you feel, especially if those expectations cause you to disregard your own needs and desires. Give yourself the gift of staying connected to yourself and your values, which becomes a much more congruent and grounded holiday experience. When we are grieving, we often ask ourselves, “when will I start to feel better?” Seasons of grief are intense and demanding in ways that we don’t experience otherwise. The emotional burden is great, our relationships may be strained as the result of our grief, and everything feels so far from normal. It is natural and normal to long for the end of these feelings. So, what does it look like to engage our grief in a way that leads to healing?
1. Learn to Tolerate and Accept the Difficult Emotions Grief requires us to befriend the most uncomfortable emotions. Grief emotions—shock, sadness, confusion, anger, longing, disorientation, despair—are all terribly uncomfortable to feel. And when our loss is significant, we end up feeling them for much longer than we ever expect. We increase our grief suffering when we fight against the grief emotions—ignoring, avoiding, overcompensating, engaging addiction—these all end up heightening our emotional experience. Additionally, when we don’t tend to our emotions, they may come out sideways in ways we don’t intend. We can help our grief process along by looking at each grief emotion that we find ourselves feeling and explore its source, its history, its message. In doing so, we are almost listening to the emotion, giving it time and space to breathe. For some, these grief emotions signal danger or threat. Take the time to disentangle these historical messages and learn to welcome each emotional character. In time each of the grief emotions will soften. 2. Notice and Name all of the Adjustments The other major focus of grief work is making many (sometimes hundreds!) of life adjustments. Without our person in our life, we may find ourselves needing to learn new skills, take on new tasks, fill new roles. Each one of these adjustments can take an enormous amount of emotional energy, during a time in life when energy is at a minimum. It is important to be aware of these adjustments, to bring them into focus by noticing and naming them. Even better, to be talking with an understanding person about them. Sometimes, we can slow the pace and take just one or two tasks or activities at a time. Other times, we just need to keep moving forward and taking care of business. Regardless, naming the many adjustments can be very helpful in processing grief and moving forward in healing. Notice for yourself how difficult these tasks feel. How are you navigating them today? Does your support system know you are working and healing in these ways? What can you request your people do for you as you engage grief healing? If you are in need of a skilled and sensitive grief therapist, please reach out to our team! We understand these tasks and are available to help create safety and opportunity for doing this work! Dialectical Behavior Therapy (DBT) offers a set of skills to help with many different emotional and relational difficulties. The four pillars of DBT are Mindfulness, Emotion Regulation, Interpersonal Effectiveness and Distress Tolerance. Each of these pillars offers a number of skills to practice in that area. I have selected three DBT skills that I believe can make a significant difference for those managing depression.
Depression is an experience that includes a slow-down or freeze response in the nervous system. People managing depression may feel numb, detached, hopeless and sad. These internal experiences may cause them to isolate from relationships, get stuck in their difficult emotions, struggle to complete normal activities. Often, those managing depression feel misunderstood by the people in their life, especially when they are encouraged to “think positively” and “just get over it.” In fact, people managing depression are often expending enormous effort to engage in their life in the most simple ways. The following set of DBT skills can be used together or individually to improve depression symptoms and help catalyze healing and forward movement. 1.Emotion Regulation Skill: Opposite Action When we are using Emotional Regulation skills, we are paying attention to whether or not our emotions fit the situation we are in. Opposite Action is a skill that we reach for when we have determined that our emotions DO NOT fit the facts of the situation. This is often the case with depression. Depression is like a lens that makes life look harder and sadder than it actually is. All emotions have an action urge, an instinctual action that the emotion makes us want to do. When our emotions DO NOT fit the situation, we benefit from acting opposite to the action urge. Here are some common emotions experienced in depression and suggestions for opposite action.
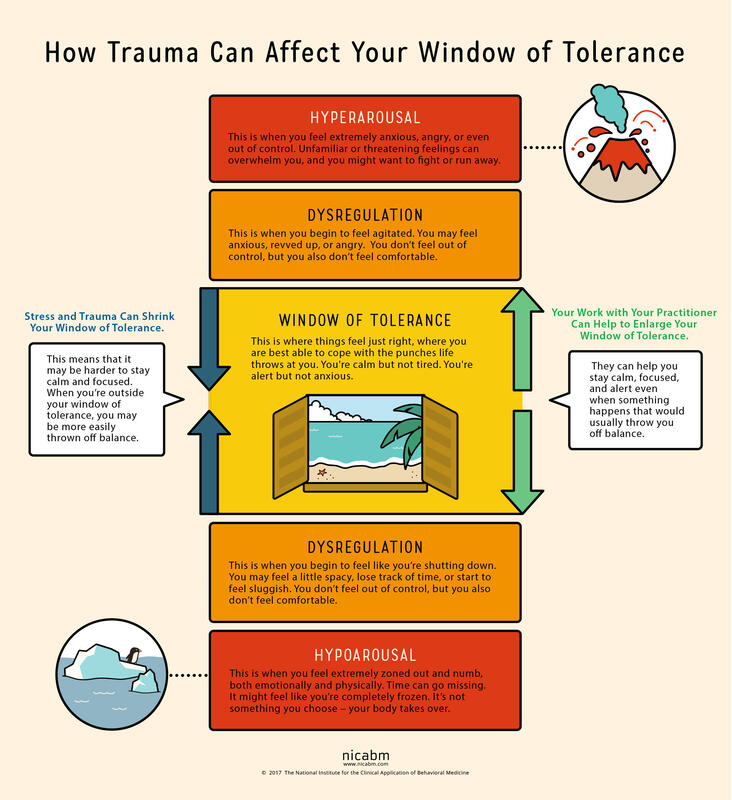
2.Interpersonal Effectiveness Skill: Making Requests Making Requests is a relationship skill that is very closely related to making boundaries. Requests highlight what we need from another person. While they can be vulnerable to make, they are also vital to communicating our needs with others. Loved ones are not mind-readers and need invitations and instructions to know how to care for those managing depression. People experiencing depression are almost always misunderstood by the people who care for them most. Unless they have experienced depression themselves, loved ones will likely minimize the depressed experience. From the outside, it may appear that it would only take a few simple steps to recover from depression. If only that were true. In order to stay connected with loved ones and to receive the care they absolutely need, those managing depression need to lean into this skill of making requests. They need to speak about how they are feeling and the effort they are expending to engage with their lives. They need to ask their loved ones to be patient with them, to use encouraging language, to offer comfort and presence rather than solutions. 3.Distress Tolerance Skill: Radical Acceptance We reach for distress tolerance skills when we are going through circumstances that are too big and/or too hard for us to change. Depression often comes on the tails of a big and hard life event, such as the loss of a loved one, a difficult transition, a painful event or unmovable circumstances. When there is truly nothing we can do to change our circumstances, we need to shift our focus toward acceptance. We are using radical acceptance skills when we work to create openness and willingness toward our difficult circumstances. Willingness is a powerful mindset shift and means that we will stop fighting against what is inevitable. Endlessly fighting against unfavorable circumstances is a recipe for suffering. Pain is inevitable in our lives, but suffering is a choice. We can still live meaningful lives in the midst of painful circumstances. When we give up the fight, we are more able to find acceptance. . . and peace. Living with depression can be a completely consuming experience. Those experiencing depression can have symptoms like persistent sadness, hopelessness, lethargy, low self-esteem, guilt, worthlessness, and more. These symptoms exist on a spectrum from mild to severe and short to long-term. Living day to day with depression feels heavy, aimless and dark. Often people suffering from depression are told to change their mindset in order to recover. We know that change must come from a much deeper place. In fact, living day to day with depression requires enormous amounts of courage and perseverance, and it helps those who are suffering to have this acknowledged and validated. Depression has several different causes and sources. There are strong inherited patterns for major depression. There are also significant hormonal impacts, especially in post-partum depression and pre-menstrual depressive disorder. Personality also has a strong influence on mood and energy and motivation. All of these different also create causes can also produce a predisposed sensitivity to depression. This blog post is to highlight when life circumstances or traumas are the source of depression. When this is the case, it is the nervous system that is leading the body and mind toward depression. And as such, treatment will need to be focused on healing the nervous system and helping the client work toward a different nervous system state. When the nervous system (read: trauma, overwhelm, life circumstances) is causing depression, healing must happen deeply in the autonomic (involuntary) nervous system. To understand the nervous system impact and the healing of nerves, we need to understand the Window of Tolerance. When we are in the window of tolerance, we are grounded, flexible and able to roll with the ups and downs of life. When we have a good amount of resilience, our window of tolerance is large and we are able to handle significant challenges without becoming too dysregulated. When we are under a lot of stress, our window of tolerance shrinks and we start to experience hyper or hypo arousal. Let’s discuss these nervous system states that exist outside of the window of tolerance. When we experience overwhelming stressors, we become dysregulated in one of two different directions, sometimes cycling between the two. We can become activated and have a flood of anxious or angry energy wash through our body (hyperaroused). Or we can become deactivated and experience numbness and a shut down response (hypoarousal). This hypoaroused state is the embodiment of depression. This is how stressors or traumas cause depression.
Hypoarousal symptoms also exist on a spectrum. On the milder side, we might experience tiredness, brain fog and a slump in energy. When hypoarousal is heightened, one might experience emotional numbness, dissociation, and even catatonia. Sometimes, we end up in this depressed state after an extended period of stress. It’s like our system is saying that it can’t handle that level of activation for that long and it shuts down. In other words, depression can be caused by a nervous system shut down. So, what does our nervous system need when it is in this shut down state? Sometimes, it simply needs a break. It needs rest from the hyper-activated state. The nerve that runs these activation pathways has become raw and overworked and needs to be soothed. The nervous system also has a significant need for connection when it is in this state of shut down. It needs a form of connection that is accepting, supportive and understanding. The nervous system also needs a way to process or integrate the overwhelming emotions that shut it down in the first place. This typically needs to happen at a slow and measured pace, so not to overwhelm again. These interventions serve as a ladder that helps us climb out of the shut down state, closer and closer to that window of tolerance. For a sustained healing process, we also need to take a good look at our lifestyle. When healing from a nervous system shut down, we need to choose a gentle pace of life, avoiding any additional stressors when possible. We can boost our nervous system health with meditation and mindfulness skills. We can invest in sustainable sleep habits that allow our entire system to regenerate every night. Gentle, joyful movement practices can also lift us out of shut down or depression. We at Benediction honor your nervous system and it’s inherent needs and functions, and we know how to move you out of harmful nervous system pathways. We can help you reconnect with yourself and with others by bringing your system back into balance in that lovely window of tolerance. |
Archives
July 2024
Categories
All
|

 RSS Feed
RSS Feed